
Who is the real ennemy? The Media or Ourselves: What Therapy approaches is effective for media-induced panic. Deciphering the mental health code.
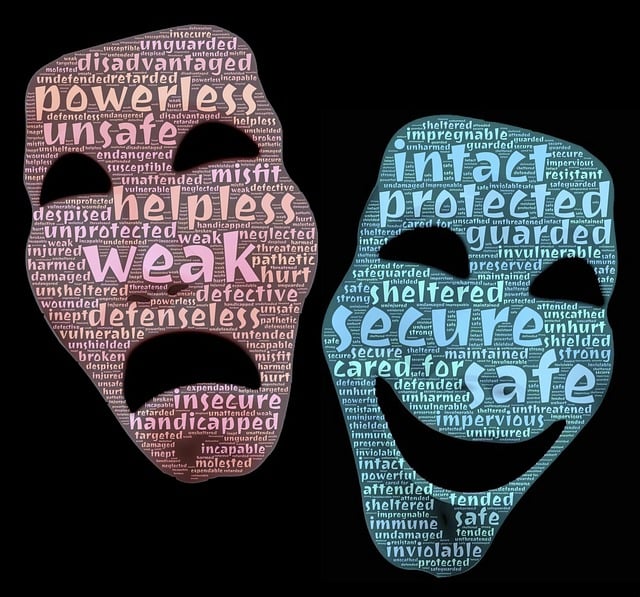
In today’s hyperconnected world, the media has become a powerful force—shaping narratives, molding opinions, and influencing emotions. News cycles, social media platforms, and online commentary often bombard us with sensationalized stories, crises, and fear-driven headlines. But the pressing question is: Who is the real enemy here—the media, or our own unguarded minds?
The answer is complex. While the media plays a role in amplifying fear, panic often takes root within us—through the way we process, internalize, and respond to this information. To understand how to protect our mental well-being in this environment, we must first understand the psychological dynamics at play.
1. How Media Fuels Panic
Media thrives on engagement. Headlines are designed to trigger emotional responses—fear, anger, shock, and urgency—because these feelings keep us scrolling and clicking. Constant exposure to alarming content activates the brain’s amygdala, the center responsible for threat detection. This can lead to:
- Heightened anxiety and hyper-vigilance
- Emotional exhaustion from constant crisis alerts
- Difficulty distinguishing fact from sensationalism
- A sense of helplessness or impending doom
This state of perceived danger is powerful. Even when the threat is not directly affecting us, our nervous system reacts as if it were—leading to a cycle of panic and overconsumption.
2. Our Role in the Cycle: The Inner Enemy
While media triggers the response, we often unconsciously feed the cycle. Doomscrolling, compulsive checking of news updates, and participating in emotionally charged online debates keep us trapped in a loop of fear. Our cognitive biases—especially negativity bias—make us more likely to focus on alarming information than on neutral or positive content.
This internalization turns external noise into internal chaos. We begin to lose control of our thought processes, allowing fear narratives to shape our worldview. In essence, the real enemy is not only the external message but also how we interpret, amplify, and react to it.
3. Therapeutic Approaches to Media-Induced Panic
Fortunately, several therapeutic approaches can help break this cycle and restore emotional balance:
a. Cognitive Behavioral Therapy (CBT)
CBT helps individuals identify distorted thinking patterns triggered by media exposure. By challenging catastrophic thoughts and reframing narratives, people learn to differentiate between actual threats and exaggerated perceptions.
b. Mindfulness-Based Stress Reduction (MBSR)
Mindfulness practices bring awareness to the present moment, reducing emotional reactivity to sensationalized news. This approach helps individuals observe information without being consumed by it.
c. Psychoeducation and Media Literacy
Therapists often incorporate psychoeducation to teach clients how media operates, why sensationalism sells, and how algorithms influence what we see. Understanding these mechanisms helps individuals detach emotionally from manipulative content.
d. Digital Detox and Exposure Control
Just as exposure therapy can help reduce phobias, intentional media breaks and boundaries help retrain the brain to not rely on constant news input for safety. Scheduling “media-free” times can significantly lower anxiety levels.
e. Somatic and Nervous System Regulation Techniques
Media panic is not just cognitive—it’s physiological. Techniques like deep breathing, grounding exercises, and movement help calm the body’s fight-or-flight response, allowing clearer thinking.
4. Deciphering the Mental Health Code
The key to managing media-induced panic isn’t about shutting out the world entirely—it’s about reclaiming agency. We cannot always control what the media shares, but we can control how we respond.
- We choose how much to consume.
- We decide which narratives to believe.
- We can build psychological tools to remain grounded.
The real enemy, then, isn’t purely the media—it’s unexamined reactivity. By understanding our mental and emotional mechanisms, we break free from panic-driven loops.
Reclaiming your inner peace by understanding what is at play here.
The world is often loud, and fear is a powerful tool used to capture attention. But your peace of mind is not something to be bought or sold. By strengthening mental health strategies, developing media literacy, and seeking therapeutic support, we can build resilience that stands firm against external chaos. It’s essential to question information thoughtfully and distinguish fact from sensationalism. History has shown that during times of crisis, narratives can become polarized, and misinformation can spread quickly. Rather than accepting everything at face value, critical thinking, credible research, and calm reflection allow us to make informed decisions. Maintaining clarity of thought is one of the strongest defenses against fear-driven narratives.
The true power lies not in what is broadcasted—but in how we choose to interpret and respond.
Learn More
The Ugly face of SAD (Seasonal Affective Disorders): Why symptoms spike in certain months and ways to alleviate them successfully.
Seasonal Affective Disorder (SAD) is more than “winter blues.” For many people it’s a recurrent, predictable pattern of mood change that can seriously disrupt work, relationships, appetite, sleep, and motivation. This article explains why symptoms spike at certain times of year, who’s at risk, and evidence-based strategies — practical, step-by-step — to reduce symptoms and regain functioning.
What is SAD?
SAD is a subtype of major depressive disorder (or, less often, a bipolar pattern) characterized by depressive episodes that recur seasonally — most commonly beginning in autumn and winter and resolving in spring. Symptoms include low mood, hypersomnia, increased appetite and carbohydrate cravings (often with weight gain), low energy, social withdrawal, and difficulty concentrating. Less commonly, some people experience summer-onset SAD with opposite features (insomnia, agitation, weight loss).
Why symptoms spike in certain months — the science, simply explained
- Reduced daylight alters circadian timing.
Shorter days in autumn/winter change the timing of the body’s internal clock (circadian rhythm). When your circadian system becomes misaligned with the local light–dark cycle, sleep and mood regulation can be disrupted. - Melatonin changes — more sleepiness, less alertness.
Melatonin (the “sleep” hormone) is produced in the dark. Longer nightly darkness can increase melatonin secretion or shift its timing, contributing to excessive sleepiness and lethargy. - Serotonin activity may drop.
Serotonin turnover in the brain has been observed to be lower in winter months in susceptible people; reduced sunlight is one factor that can lower serotonin function and contribute to depressive symptoms. - Photoperiod sensitivity and latitude effects.
The likelihood and severity of SAD rise with latitude: the farther from the equator, the bigger seasonal shifts in daylight, and the higher the SAD rates. Photoperiod (day length) appears to be a key trigger for people who are sensitive to these changes. - Behavioral and social factors.
Colder, darker months often bring reduced outdoor activity, less socializing, increased sedentary time, and dietary shifts — all of which can worsen mood. Holiday stress and disrupted routines can also compound vulnerability.
When do symptoms typically spike?
In the northern hemisphere, most cases begin in late autumn and are worst December–February, resolving by spring. (In the southern hemisphere the pattern is reversed.) A small minority experience summer-onset SAD with different triggers (heat, longer days).
Who’s at higher risk?
- People living at higher latitudes (less winter daylight).
- Those with a prior history of major depressive episodes that are seasonal.
- Women are diagnosed more often than men (possible combinations of biological and help-seeking differences).
- Individuals with family history of mood disorders.
- People who have other risk factors such as vitamin D deficiency, disrupted sleep, or social isolation.
Evidence-based treatments and practical steps
Below are treatments supported by research. Many people use combinations (e.g., light therapy + CBT) for faster and more durable benefit.
1) Bright light therapy (first-line for winter SAD)
- What it is: Sitting near a specially designed “light box” that delivers bright, diffuse light (not a tanning lamp) early each morning. It mimics outdoor morning light and re-entrains the circadian system.
- Typical regimen used in trials: 10,000 lux, ~16–60 cm (about 16 inches) from the face, for about 20–30 minutes each morning, ideally within 30–60 minutes of waking. Consistency every day (including weekends) matters. Start before symptoms become severe for best prevention.
- Practical tips: Sit reading or having coffee while using the box; don’t stare directly into the light; position it slightly to the side so light enters the eyes indirectly. If 10,000 lux is impractical, longer durations at lower lux can help — but follow device instructions.
- Safety: Light therapy is generally safe; common side effects are eye strain, headache, or jitteriness. People with bipolar disorder need close monitoring (risk of inducing mania). Ask your clinician before starting if you have eye disease or take photosensitizing medication.
2) Cognitive-Behavioral Therapy tailored for SAD (CBT-SAD)
- What it does: Combines standard CBT techniques (behavioral activation, cognitive restructuring) with modules addressing seasonal triggers and relapse prevention. Trials show CBT-SAD works as well as light therapy acutely and may reduce recurrence rates longer term.
- Practical format: Weekly sessions for 8–12 weeks with homework assignments (scheduling activities, addressing negative seasonal thinking). Consider CBT-SAD if you prefer psychotherapy or want longer-term protection against recurrence.
3) Medication — particularly bupropion XL for prevention
- What the evidence says: Bupropion XL (sustained-release bupropion) has FDA labeling for prevention of seasonal major depressive episodes in patients with a history of SAD. Other antidepressants (SSRIs) are also effective for acute treatment. Discuss options with a prescriber.
- How it’s used clinically: Some people begin prophylactic medication in autumn to prevent a seasonal episode; others treat acutely and taper in spring under medical guidance. Always consult a prescriber for suitability, dosing, and side-effect management.
4) Lifestyle interventions (essential adjuncts)
- Maximize natural daylight: Spend 20–30 minutes outside each morning when possible — even on cloudy days the outdoor light is much brighter than indoor lighting.
- Exercise: Regular aerobic exercise reduces depressive symptoms and counteracts lethargy. Aim for 30 minutes most days.
- Sleep hygiene: Keep a consistent wake time (very important for circadian stability); avoid long daytime naps; limit evening bright light from screens.
- Diet: Choose balanced meals, emphasize whole foods, protein to stabilize blood sugar, and moderate carbohydrate choices to manage cravings. Omega-3s and a diet with adequate nutrients may help mood.
- Social activation: Plan regular social commitments and structure during winter to counter withdrawal.
5) Check and correct medical contributors
- Vitamin D: Low vitamin D is common in winter and may worsen mood for some people. Test serum 25-OH vitamin D if suspected; supplementation strategies should be individualized and discussed with your clinician.
- Thyroid and other medical screens: Hypothyroidism and other medical conditions can mimic or worsen depression; rule these out with your provider.
6) Preventive planning (best practice)
- If you have a history of SAD, plan ahead: start light therapy or your agreed preventative strategy in early autumn or at the first sign of symptoms. Proactive plans reduce the chance of a severe episode. Trials suggest starting prophylactic bupropion XL or beginning light therapy early can reduce recurrence.
A practical 6-week plan (example)
Week 0 (late autumn, ideally before symptoms peak)
- Obtain a medical check (vitamin D, thyroid) and discuss history with your clinician. Consider ordering a medically approved 10,000-lux light box.
Weeks 1–2
- Begin light therapy: 10,000 lux for 20–30 minutes each morning within 30–60 minutes of waking.
- Add 3x/week brisk walking outdoors (20–30 minutes).
- Implement consistent wake time and sleep hygiene.
Weeks 3–6
- If symptoms improve → continue. If partial response → add CBT-SAD or psychotherapy and/or discuss medication with prescriber.
- Keep activity scheduling, social contacts, and daylight exposure.
(Adjust based on response and clinician guidance.)
When to seek professional help
- Symptoms are severe, suicidal thoughts occur, or you can’t carry out daily responsibilities — seek immediate professional help.
- If self-help and lifestyle changes aren’t improving symptoms after 2–4 weeks, consult your primary care doctor or mental health professional about adding CBT or medication.
Common myths — corrected
- Myth: SAD is “just” feeling a bit down in winter.
Reality: SAD can be a clinically significant, recurrent depressive disorder that impairs function and benefits from targeted treatment. - Myth: You simply need more willpower.
Reality: Biological shifts in light exposure, neurotransmitters, and circadian timing are real contributors; combining biological and behavioral treatments is most effective.
Final Thoughts and perspective to SAD
SAD is a predictable, biologically influenced condition for many people. The “ugly face” of SAD is the sudden, seasonal drop in energy, mood, and functioning — but the good news is that effective, evidence-based strategies exist: morning bright-light therapy, CBT-SAD, medication options (including bupropion XL for prevention), and everyday lifestyle measures. If you or someone you care about experiences a consistent pattern of seasonal depression, plan early, consult a clinician, and use a combination approach — prevention dramatically improves outcomes.
Learn More
The Many Facets of Anxiety: How It Manifests as Irritability or Anger and Managing Them for a Happier, Serene Life
Anxiety is a complex and often misunderstood emotion. While most people associate it with worry, panic attacks, or restlessness, anxiety can also wear the mask of irritability or even anger. This disguised form can wreak havoc on our relationships, peace of mind, and overall well-being if not properly understood and managed.
Let’s dive into how anxiety shows up in unexpected ways, why it morphs into irritability or anger, and how we can address it for a more balanced, joyful life.
Understanding the Nature of Anxiety
Anxiety is the body’s response to perceived danger or stress. It triggers the “fight, flight, or freeze” response and prepares us to react. While this mechanism is essential for survival, it becomes problematic when overactivated by everyday stressors—deadlines, relationships, finances, health concerns.
When anxiety becomes chronic, it stops being helpful and starts manifesting in less obvious, but equally destructive ways.
Why Anxiety Turns into Irritability or Anger
Though they seem like separate emotions, anxiety and anger are closely linked:
- Overstimulation: When your brain is in constant overdrive from worry or hypervigilance, you’re more likely to become frustrated or overwhelmed quickly.
- Perceived Threats: Anxiety can cause you to interpret neutral events as threats. This leads to a defensive, sometimes aggressive reaction.
- Lack of Control: Feeling out of control is deeply unsettling. That discomfort can easily morph into anger, especially when we feel helpless.
- Bottled-up Emotions: When anxiety is suppressed, it can come out sideways—as sarcasm, short-temperedness, or even rage.
In truth, many people who seem “angry” are often silently struggling with underlying anxiety.
How to Recognize the Signs
You might be experiencing anxiety-related irritability or anger if you:
- Feel unusually impatient or snap at others over minor issues
- Notice a short fuse in stressful situations
- Experience muscle tension, headaches, or clenched jaws
- Constantly feel “on edge” or overly alert
- Regret reactions that felt disproportionate afterward
Acknowledging these patterns is the first step toward regaining inner calm.
Strategies for Managing Anxiety-Driven Irritability and Anger
- Pause and Breathe
Deep breathing activates the parasympathetic nervous system, calming your fight-or-flight response. Practice box breathing: inhale for 4 seconds, hold for 4, exhale for 4, and hold for 4 again.
- Identify Triggers
Journaling or reflecting on moments when you felt irritable can help pinpoint recurring triggers. Is it work-related? A particular person? Lack of sleep?
- Reframe Your Thoughts
Anxiety often stems from distorted thinking. Catch yourself in moments of catastrophizing or assuming the worst. Replace fear-driven thoughts with balanced, empowering ones.
- Use Physical Activity as an Outlet
Movement releases pent-up energy and boosts feel-good endorphins. Even a brisk walk can dissipate rising frustration.
- Practice Mindfulness and Meditation
These tools train your mind to stay present, reducing rumination and reactivity. Over time, they build emotional resilience.
- Communicate Openly
Let others know what you’re experiencing. Saying, “I’m feeling overwhelmed, I need a moment,” is far healthier than letting tension explode later.
- Seek Professional Support
Therapy—especially cognitive behavioral therapy (CBT)—can be transformative in understanding and reshaping anxiety’s impact on your emotional responses.
Living a More Serene Life
Healing from anxiety-induced irritability is not about becoming emotionless; it’s about gaining mastery over your responses. When you understand the roots of your reactions, you stop being ruled by them. You move from reactive to responsive, from chaotic to centered.
Imagine waking up not bracing for the day, but embracing it. Imagine conversations filled with patience instead of tension. That serenity isn’t just a dream—it’s a skill. And like all skills, it grows with intention and practice.
Mother nature of anxiety: From Storm to Stillness
Anxiety is not your enemy. It’s a messenger—alerting you to unresolved fears, unmet needs, or unsustainable stress levels. When we listen with compassion, not judgment, we can transform our anxiety from a source of pain into a catalyst for growth.
Let every day be a chance to pause, breathe, and choose peace over panic, understanding over outbursts, and joy over fear.
Because within every anxious heartbeat lies the quiet potential for a calm, powerful, and radiant life.
Concluding words of wisdom: “You’re not broken—you’re becoming. And every moment of awareness is a step closer to the peace you deserve.”

How Expressing Vulnerability in a Relationship Can Help Build Deeper Connection: Understanding the Distinction Between Weakness and Strength
In today’s fast-paced and often emotionally guarded world, the concept of vulnerability is frequently misunderstood. Particularly in romantic relationships, vulnerability can be mistaken for weakness, dependency, or being “too emotional.” In some circles, especially among men, it’s even equated with being a “Simp”—a derogatory term used to describe someone perceived as overly submissive or eager to please their partner. But the truth is, genuine vulnerability is a profound strength. It has the power to deepen trust, foster emotional intimacy, and create a lasting foundation of love and understanding.
This new article explores how expressing vulnerability in a relationship can build a deeper connection, and why it is far from being weak or “simp-like.” Rather, it is a courageous act of authenticity, maturity, and emotional intelligence.
What is Vulnerability in a Relationship?
Vulnerability in a relationship is the willingness to be open and honest about your thoughts, feelings, needs, and fears—even when doing so feels uncomfortable or uncertain. It means dropping your guard, removing your emotional armor, and trusting your partner with the real you, not just the curated, polished version of yourself.
This could involve:
- Admitting fears of inadequacy or rejection
- Expressing needs for reassurance or affection
- Opening up about past trauma or insecurities
- Saying “I love you” first
- Apologizing sincerely after a mistake
- Asking for help or support
These acts of vulnerability demonstrate authenticity and a deep level of self-awareness. They invite your partner into your inner world and build a space where both people can be seen and accepted without judgment.
The False Link Between Vulnerability and Weakness
Modern society often glorifies independence, stoicism, and emotional self-sufficiency, especially for men. This conditioning leads many to believe that expressing emotions or needs is a sign of weakness. The term “simp” has become part of pop culture lingo to mock individuals who are openly affectionate, caring, or emotionally available—suggesting that loving deeply or showing vulnerability makes one less respected or less masculine.
But nothing could be further from the truth. Vulnerability is not about begging for attention or surrendering your boundaries. It is not about losing yourself in someone else or prioritizing their happiness above your own to your detriment. True vulnerability is an act of bravery. It takes far more strength to be open and emotionally honest than it does to hide behind silence or emotional detachment.
In fact, people who are comfortable being vulnerable demonstrate emotional resilience. They are secure enough in themselves to acknowledge their needs, admit their flaws, and risk rejection in pursuit of genuine connection. That is not weakness—that is strength.
How Vulnerability Builds Deeper Connection
1. Creates Emotional Intimacy
Surface-level conversations and interactions can only sustain a relationship for so long. Emotional intimacy is what makes a bond meaningful and lasting. Vulnerability fosters this intimacy by encouraging deeper understanding and empathy between partners. When you let your guard down and share your inner experiences, your partner sees the real you, which invites them to do the same. This mutual sharing creates a bond that is rich, honest, and deeply connected.
2. Builds Trust
Trust is essential in any relationship, and vulnerability is one of the key ways to build and reinforce it. When you are vulnerable with your partner, you are saying, “I trust you with my heart.” This openness often encourages reciprocation, establishing a safe emotional space where both individuals can be themselves without fear of judgment.
3. Enhances Communication
When couples avoid vulnerability, communication often becomes superficial or defensive. Vulnerability opens the door for honest, non-defensive dialogue. It allows you to speak from the heart, express unmet needs, and navigate conflicts with empathy and understanding. Vulnerable communication invites collaboration instead of confrontation.
4. Encourages Growth and Healing
Everyone carries emotional wounds, insecurities, and fears. In a healthy relationship, vulnerability allows for those wounds to be seen and healed. Being open about your struggles invites compassion and support, both of which are critical for personal and relational growth. Vulnerability can also help break toxic patterns and build healthier dynamics.
5. Strengthens Commitment
When partners can be vulnerable with each other, they often feel more bonded and committed. Vulnerability signals emotional investment. It tells your partner, “You matter to me enough for me to take this emotional risk.” This kind of transparency strengthens the commitment to weather challenges together and deepen the emotional connection.
Practical Ways to Practice Healthy Vulnerability
If vulnerability doesn’t come naturally, the good news is that it can be developed. Here are a few practical strategies to help you embrace vulnerability in your relationship:
- Start Small: You don’t have to reveal everything at once. Begin with small, honest expressions of how you feel and build from there.
- Use “I” Statements: Express your feelings using “I” statements, like “I feel anxious when I don’t hear from you,” rather than blame-based language.
- Be Honest About Your Needs: Whether it’s needing reassurance, physical affection, or time alone, articulating your needs is a key part of vulnerability.
- Share Your Fears: Talk about your insecurities or past experiences that shape how you relate. It builds empathy and understanding.
- Practice Active Listening: Show your partner that you value their vulnerability too by listening without interrupting, judging, or trying to fix everything.
Redefining Masculinity and Strength
One of the biggest shifts needed in modern relationships is redefining what it means to be strong. Masculinity, in particular, has long been associated with emotional stoicism, dominance, and control. But true strength lies in being fully human—in owning your emotions, expressing love without shame, and showing up authentically in your relationships.
It’s time to move beyond outdated stereotypes and embrace a more inclusive, emotionally intelligent view of strength. Men who are vulnerable are not weak; they are brave. They are the kind of partners who build lasting, meaningful relationships because they lead with heart, not ego.
The Balance: Vulnerability with Boundaries
Of course, vulnerability doesn’t mean sharing everything indiscriminately or losing your sense of self. Healthy vulnerability includes boundaries. It involves being intentional about what you share and ensuring that your openness is met with respect and mutual care.
If you find that your vulnerability is consistently dismissed, mocked, or weaponized in your relationship, that is not a safe or healthy space. Vulnerability should be met with empathy, not exploitation. Choosing to be vulnerable should always include choosing people who are emotionally safe.
Vulnerability is Strength
Expressing vulnerability in a relationship is one of the most courageous and impactful things you can do. It builds trust, deepens emotional connection, enhances communication, and fosters growth. It allows both partners to be fully seen, accepted, and loved for who they truly are.
Being vulnerable doesn’t make you a simp or weak. It makes you real. It makes you human. And most importantly, it makes you a better partner.
So the next time you feel the urge to hold back out of fear of looking weak, remember: vulnerability isn’t about losing power—it’s about sharing it. And in that mutual sharing lies the foundation for the kind of love that lasts.


How can proper therapy help children of couples going through separation or divorce. The short and long term impact of broken families on children and their present behaviors inside and outside of school.
Separation and divorce are emotionally challenging experiences for families, particularly for children. The instability and emotional turmoil associated with a family breakup can significantly affect a child’s mental, emotional, and social well-being. However, proper therapy plays a crucial role in helping children navigate this difficult transition, providing them with coping mechanisms that can mitigate both short- and long-term negative effects. Let’s first discuss the short term effect on children when parents separate or divorce
Short-term effects of separation/divorce on children
The immediate impact of divorce on children can manifest in various ways, depending on their age, personality, and the level of conflict between parents. Some of the common short-term effects include:
1. Emotional distress
- Feelings of confusion, sadness, anger, guilt, or anxiety are prevalent.
- Fear of abandonment or concerns about stability can arise.
- Mood swings and emotional outbursts may occur as children struggle to process the change.
2. Behavioral changes
- Increased irritability, aggression, or defiance toward authority figures.
- Withdrawal from family and social activities.
- Difficulty concentrating on schoolwork and extracurricular activities.
3. Academic decline
- Decreased motivation and lower academic performance.
- Struggles with focus and attention due to emotional distress.
- Increased absenteeism or disinterest in school activities.
4. Social struggles
- Difficulty maintaining friendships due to feelings of isolation.
- Potential trust issues, making it harder to form new bonds.
- Increased dependence on one parent while distancing from the other.
Long-term effects of separation/divorce:
If not properly addressed, the impact of a broken family can extend into adulthood. Long-term consequences include:
1. Emotional and psychological struggles
- Higher risk of anxiety and depression.
- Difficulty managing emotions in future relationships.
- Fear of commitment and trust issues in personal relationships.
2. Poor relationship patterns
- Increased likelihood of experiencing relationship conflicts or divorces in their own future marriages.
- Struggles with attachment and intimacy due to unresolved childhood trauma.
3. Academic and career setbacks
- Lower self-esteem and confidence may hinder academic and career success.
- Increased likelihood of dropping out of school or underachieving.
- Difficulty in handling workplace relationships and professional growth.
4. Risky behavior and substance abuse
- Higher probability of engaging in risky behaviors such as drug or alcohol abuse.
- Increased chances of engaging in delinquent activities.
- Potential difficulty in managing stress and peer pressure.
How therapy helps children cope with separation/divorce
Proper therapy offers children a safe space to express their emotions, understand their situation, and develop healthy coping mechanisms. Some of the key benefits of therapy include:
1. Emotional expression and validation
- Encourages children to talk about their feelings in a non-judgmental environment.
- Helps them understand that their emotions are valid and normal.
- Assists in reducing guilt or self-blame associated with the divorce.
2. Building coping skills
- Equips children with tools to manage anxiety, sadness, and anger.
- Teaches relaxation techniques such as mindfulness and deep breathing.
- Provides problem-solving skills to handle stress and uncertainty.
3. Strengthening parent-child relationships
- Family therapy can help parents and children communicate more effectively.
- Encourages parents to co-parent in a way that prioritizes the child’s well-being.
- Helps parents understand their child’s perspective and emotions.
4. Enhancing academic and social performance
- Therapists work with children to improve concentration and motivation in school.
- Social skills training can help children rebuild friendships and trust.
- Therapy provides strategies to adapt to new family dynamics and school environments.
5. Preventing long-term psychological impact
- Early intervention reduces the likelihood of future mental health issues.
- Therapy fosters resilience, teaching children how to adapt to change positively.
- Encourages self-confidence and a positive outlook on relationships and family.
Types of therapy beneficial for children of divorce
1. Individual therapy
A licensed therapist works one-on-one with the child to address emotional distress, behavioral changes, and coping strategies tailored to their needs.
2. Family therapy
Helps improve communication between parents and children, ensuring that all family members understand and support one another during the transition.
3. Group therapy
Allows children to interact with peers who are also experiencing parental separation, helping them feel less isolated and providing shared coping strategies.
4. Play therapy (For Younger Children)
Engages children in play-based activities that allow them to express emotions non-verbally and process their experiences in a way that feels natural to them.
5. Cognitive Behavioral Therapy (CBT)
Helps children identify and challenge negative thoughts, replacing them with positive thinking patterns and effective coping mechanisms.
Divorce can have profound short- and long-term effects on children, but proper therapy provides them with the support they need to cope with emotional distress, build resilience, and maintain healthy relationships. By investing in professional therapy, parents can help their children navigate this challenging period and ensure a healthier, more stable future. Ultimately, prioritizing a child’s emotional and psychological well-being during a family breakup can make all the difference in their ability to thrive despite the challenges they face.


Carrying the weight of depression symptoms due to loneliness. How to break the isolation cycle post pandemic. Effective strategies that can help you get back into society and mingle with other human beings.
The COVID-19 pandemic reshaped social interactions, forcing many into prolonged isolation. As a result, countless individuals found themselves struggling with loneliness, which has contributed to depression symptoms such as persistent sadness, fatigue, loss of interest, and anxiety. The absence of regular human connection can deepen feelings of despair, making it even harder to reintegrate into society. However, breaking the cycle of isolation is essential for improving mental well-being. Here are effective strategies to help you reconnect with others and reclaim a fulfilling social life.
Understanding the Link Between Loneliness and Depression
Loneliness and depression are intricately connected, forming a cycle that can be difficult to break. While loneliness is the emotional distress caused by a lack of meaningful social connections, depression is a more pervasive mental health condition that affects mood, energy levels, and overall well-being. When left unaddressed, loneliness can contribute to the onset of depression, and in turn, depression can cause individuals to further isolate themselves, deepening feelings of loneliness.
How Loneliness Contributes to Depression
- Lack of Social Support – Human beings are inherently social creatures, and strong relationships play a crucial role in mental health. When someone lacks companionship, they may feel unimportant or disconnected, which can lead to feelings of sadness and hopelessness.
- Increased Negative Thinking – Without external perspectives from friends or family, lonely individuals may develop negative thought patterns. They may believe they are unworthy of companionship or assume others do not care about them, reinforcing depressive thoughts.
- Reduced Dopamine and Serotonin Levels – Social interaction stimulates neurotransmitters like dopamine and serotonin, which regulate mood and emotions. A lack of connection can disrupt this balance, making loneliness a biological trigger for depression.
- Loss of Purpose and Motivation – Many social activities provide a sense of purpose. When someone withdraws from social engagement, they may experience a decline in motivation, leading to further isolation and worsening depressive symptoms.
- Chronic Stress and Anxiety – Loneliness can increase cortisol levels, the stress hormone, which negatively impacts both mental and physical health. Persistent stress contributes to anxiety, making social situations even more intimidating for those already struggling.
How Depression Reinforces Loneliness
- Social Withdrawal – A key symptom of depression is the tendency to withdraw from social interactions. The more someone avoids socializing, the more disconnected they become, deepening their loneliness.
- Loss of Interest in Activities – Depression often causes people to lose interest in hobbies or events they once enjoyed, making it difficult to engage with others. This leads to fewer social opportunities and increased isolation.
- Feelings of Shame or Unworthiness – Those with depression may feel like a burden to others, leading them to avoid seeking help or initiating social interactions. They may believe that others won’t understand or that they don’t deserve companionship.
- Fatigue and Low Energy – The mental and physical exhaustion caused by depression can make even simple social activities feel overwhelming. As a result, individuals may avoid contact with friends and family, further exacerbating loneliness.
Strategies on breaking that vicious cycle: Steps Toward Healing
Reentering society after a long period of isolation can be daunting, but taking small, intentional steps can help ease the transition. Here are some practical ways to reconnect with the world and find happiness from within:
1. Start Small and Gradual
Reintegrating into social settings doesn’t mean jumping into large crowds immediately. Begin by engaging in low-pressure interactions, such as short conversations with neighbors, cashiers, or acquaintances. Small social interactions can help build confidence and make the idea of larger gatherings less intimidating.
2. Join Community Groups or Clubs
Finding a shared interest is a great way to make new connections. Consider joining a book club, art class, or fitness group. Many communities offer support groups for those struggling with loneliness and mental health challenges, providing a safe space to interact with others who understand your experience.
3. Reconnect with Old Friends and Family
Sometimes, loneliness persists because we have lost touch with those we once cared about. Reaching out to an old friend or a family member can rekindle relationships that provide comfort and support. A simple text or phone call can be the first step toward rebuilding social ties.
4. Volunteer Your Time
Volunteering provides a sense of purpose and a structured way to interact with others. Helping out at a local charity, animal shelter, or community center can create new connections while also giving you a reason to engage with the world in a meaningful way.
5. Seek Professional Support
If loneliness has contributed to severe depression, seeking help from a therapist or counselor is crucial. Cognitive-behavioral therapy (CBT) and other therapeutic approaches can help you navigate feelings of isolation, identify negative thought patterns, and develop coping mechanisms for social anxiety.
6. Use Technology to Your Advantage
While excessive screen time can contribute to isolation, technology can also be a useful tool for reconnecting with others. Virtual meetups, online support groups, and social media platforms can help bridge the gap until you feel comfortable engaging in face-to-face interactions.
7. Set Small, Achievable Social Goals
Instead of pressuring yourself to make drastic changes overnight, set small, realistic goals. This could be as simple as having one conversation per day, attending a local event, or inviting a friend for coffee. Celebrate each step as a victory to build momentum and confidence.
8. Engage in Physical Activity
Exercise has been shown to improve mood and reduce symptoms of depression. Activities such as yoga, group fitness classes, or even a daily walk in a public space can provide opportunities to be around others without the pressure of direct interaction.
Loneliness doesn’t have to lead to permanent depression—unless you let it. We have the power to control how external challenges affect us, both in the short and long term. We can either confront and overcome them or allow them to break us. Life presents us with choices, and it’s up to us to face the obstacles ahead.
Escaping the cycle of isolation takes time and effort, but the rewards are life-changing. Human connection is essential for emotional well-being, and by taking small, intentional steps, you can rediscover the fulfillment of meaningful relationships. You’re not alone—many are navigating post-pandemic loneliness alongside you. Be patient, seek support when needed, and move forward at your own pace.
With persistence and the right approach, you can rebuild your social life and experience the joy of true connection once again.


Strengthening Resilience: Several effective strategies to protect your mental health from the many downsides of anxiety disorder
Anxiety is a natural reaction to stress, but when it becomes persistent or overwhelming, it can take a toll on both mental and physical health. Strengthening resilience is key to managing anxiety and fostering a healthy, balanced mind. Resilience doesn’t mean avoiding stress—it’s about developing the ability to adapt and bounce back from life’s challenges.
This article explores several effective strategies to build resilience and protect mental well-being from the effects of anxiety disorder. Keep in mind that not every approach will work for everyone, but by gaining insight and understanding, you may discover techniques that suit you best. Let’s explore them one by one.
1. Develop a Growth Mindset
A growth mindset is the belief that abilities and intelligence can be developed through dedication and hard work. Viewing challenges as opportunities to grow rather than threats can shift your perspective and reduce anxiety. Embrace setbacks as learning experiences, and remind yourself that difficulties are temporary and surmountable.
2. Practice Mindfulness and Meditation
Mindfulness involves focusing on the present moment without judgment. Regular mindfulness practice can help reduce anxiety by shifting attention away from distressing thoughts and fostering a sense of calm. Meditation, deep breathing, and body scanning techniques can further support emotional regulation and stress management.
3. Prioritize Self-Care
Taking care of your body and mind is crucial in strengthening resilience. Ensure you get adequate sleep, maintain a balanced diet, and engage in regular physical activity. Exercise, in particular, has been shown to reduce anxiety by releasing endorphins and improving mood. Additionally, engaging in activities that bring joy and relaxation, such as hobbies or spending time in nature, can contribute to overall mental well-being.
4. Build a Strong Support System
Having supportive relationships can significantly buffer the effects of anxiety. Surround yourself with positive and understanding individuals who encourage resilience. Whether through family, friends, support groups, or therapy, meaningful connections provide comfort and guidance during stressful times.
5. Cultivate Emotional Regulation Skills
Managing emotions effectively can prevent anxiety from escalating. Techniques such as journaling, cognitive reframing, and engaging in creative outlets like art or music can help process emotions in a healthy way. Identifying triggers and developing coping mechanisms tailored to your needs can also enhance emotional resilience.
6. Establish Healthy Boundaries
Setting boundaries is essential for maintaining mental health and preventing burnout. Learn to say no to demands that exceed your emotional or physical capacity. Prioritize activities that align with your well-being, and avoid situations or individuals that contribute to unnecessary stress.
7. Develop Problem-Solving Skills
Resilience involves facing problems head-on rather than avoiding them. Strengthen your problem-solving skills by breaking challenges into manageable steps. Identify possible solutions, weigh their pros and cons, and take action. Feeling in control of situations can reduce anxiety and enhance confidence in handling future stressors.
8. Seek Professional Help When Needed
There is no shame in seeking professional support when anxiety becomes overwhelming. Therapy, counseling, or psychiatric intervention can provide tailored strategies and coping mechanisms. Cognitive-behavioral therapy (CBT), in particular, has proven effective in reducing anxiety symptoms and improving resilience.
Building resilience against anxiety disorder requires consistent effort and self-awareness. By fostering a growth mindset, practicing mindfulness, prioritizing self-care, and seeking support, you can strengthen your mental health and navigate life’s challenges with confidence. Remember, resilience is not about eliminating stress but about developing the capacity to adapt, recover, and thrive

The many ugly outcome of generational trauma: Effective strategies on how to reclaim full control of your thoughts after dealing with any sorts of trauma. Secrets revealed.
Generational trauma, also referred to as intergenerational or transgenerational trauma, is a deeply rooted phenomenon that manifests as the lingering psychological effects of a traumatic event passed down from one generation to the next. This trauma doesn’t just affect individuals—it ripples through entire families and communities, shaping behaviors, relationships, and mental health outcomes. From substance abuse and anxiety disorders to unhealthy relationship patterns and self-destructive tendencies, the outcomes of generational trauma can be devastating. But there is hope. With effective strategies, you can reclaim control of your thoughts and heal from the impact of trauma.
Understanding Generational Trauma: What It Is and How It Shapes Us
Generational trauma stems from unresolved pain or distress experienced by ancestors. Examples include surviving genocide, systemic racism, war, abuse, or poverty. While the initial trauma occurs in the past, its effects are transmitted through parenting styles, family dynamics, and even epigenetic changes—alterations in how genes are expressed.
The outcomes of generational trauma include:
- Emotional Dysregulation: Difficulty managing emotions, leading to anger outbursts, anxiety, or depression.
- Trust Issues: Fear of vulnerability, often causing relationship problems or isolation.
- Low Self-Worth: Feelings of inadequacy rooted in inherited beliefs.
- Self-Sabotaging Behaviors: Engaging in actions that hinder personal growth, often subconsciously.
- Perpetuation of Abuse: Normalization of harmful behaviors, passed down as learned coping mechanisms.
These patterns are often unconscious, making them difficult to identify without self-awareness and intentional work.
Reclaiming Control of Your Thoughts After Trauma
Healing from trauma requires a multifaceted approach. Below are effective strategies to help you regain control of your mind and break free from the cycle of generational trauma.
1. Acknowledge the Trauma
- The first step to healing is recognition. Identify the patterns in your family or your own behaviors that might stem from generational trauma. Journaling, reflecting on family stories, or speaking with a therapist can help uncover these links.
- Tip: Explore family narratives with curiosity, not blame. Understanding the origin of trauma can empower you to confront it.
2. Seek Professional Help
- Therapists trained in trauma recovery (such as EMDR practitioners or those using somatic experiencing) can help you process deep-seated pain. Therapy provides a safe space to explore your emotions, unpack inherited patterns, and develop healthier coping mechanisms.
- Support groups can also connect you with others who understand your struggles, fostering shared healing.
3. Practice Mindfulness
- Trauma often hijacks the mind, leading to intrusive thoughts and hypervigilance. Mindfulness techniques like meditation, deep breathing, and body scans help you stay grounded in the present.
- Exercise: Try the “5-4-3-2-1 Technique” to calm racing thoughts by naming five things you can see, four you can touch, three you can hear, two you can smell, and one you can taste.
4. Challenge Negative Beliefs
- Trauma plants seeds of self-doubt and fear. Rewriting your internal dialogue is essential to healing.
- Cognitive Behavioral Therapy (CBT) can help identify and replace negative thought patterns with empowering ones.
- Example Affirmation: “I am worthy of love and respect, regardless of my past or family history.”
5. Set Boundaries
- Breaking the cycle of trauma often requires establishing firm boundaries with toxic individuals. While difficult, this step can protect your mental well-being and pave the way for healthier interactions.
- Tip: Start small. Practice saying “no” or voicing your needs in situations where you feel unsafe or overwhelmed.
6. Reconnect with Your Body
- Trauma often disconnects us from our physical selves. Activities like yoga, tai chi, or dance can restore this connection by releasing tension stored in the body.
- Pro Tip: Journaling alongside body-focused practices can deepen self-awareness by revealing emotional patterns linked to physical sensations.
7. Explore Your Family History with Compassion
- Reframing how you see your ancestors’ struggles can help you break the cycle without resentment. This doesn’t mean excusing harmful behaviors—it means understanding how trauma shaped their actions and resolving to do better.
- Action Step: Create a “family resilience map” that highlights not just the trauma but also the strengths and survival skills passed down.
8. Cultivate Gratitude and Joy
- Trauma narrows focus on pain, but gratitude helps rewire the brain to notice positives. Write down three things you’re grateful for daily. Seek out moments of joy, however small, and let them anchor you in hope.
9. Engage in Creative Outlets
- Expressive activities like painting, writing, or music provide a safe outlet to process emotions. Creative pursuits can help uncover buried feelings and turn pain into purpose.
10. Forgive Yourself and Others
- Forgiveness doesn’t mean condoning harm but releasing its hold on you. Start with self-forgiveness—letting go of guilt or shame tied to inherited patterns.
Secrets to Long-Term Healing
- Break the Silence: Generational trauma often thrives in secrecy. Open conversations within your family, even if uncomfortable, can disrupt the cycle.
- Embrace Resilience: Remember, your ancestors survived unimaginable struggles. Their resilience flows within you, equipping you to break the chains of trauma.
- Focus on Growth: Healing isn’t linear. Celebrate small victories and remain patient with setbacks.
- Pay It Forward: As you heal, share your journey. By breaking the stigma around trauma, you inspire others to embark on their own paths to recovery.
Here are my final Thoughts on this topic: How to reclaim your power
Generational trauma may have shaped your past, but it doesn’t have to define your future. Through acknowledgment, professional help, and intentional healing practices, you can reclaim control of your thoughts and break free from inherited patterns. By confronting and transforming this pain, you not only heal yourself but also create a legacy of hope and resilience for generations to come.
Healing is possible—and it starts with you. Take the first step today.


Complexities of S.A.D (Seasonal Affective Disorders): Coping with mood disorders related to winters and cold temperatures. Effective Strategies that can work during these long winter months to alleviate these moods.
Seasonal Affective Disorder (SAD) is a type of mood disorder that recurs seasonally, often in winter when daylight hours are reduced. The symptoms of SAD are similar to those of major depressive disorder and may include persistent low mood, fatigue, irritability, sleep problems, overeating, and social withdrawal. Those affected by SAD can find it difficult to maintain motivation and experience a general decline in well-being.
Here’s a detailed exploration of SAD, the science behind it, and effective strategies for coping during the winter months.
1. Understanding SAD: Causes and Biological Mechanisms
- Light and Melatonin Regulation: Reduced sunlight in winter affects our circadian rhythms, which are regulated by light. This can lead to overproduction of melatonin, the hormone that regulates sleep, causing drowsiness and lethargy during waking hours.
- Serotonin Production: Low sunlight exposure may lower serotonin levels in the brain. This neurotransmitter is crucial for mood stabilization, and lower levels can lead to feelings of depression and lethargy.
- Vitamin D Deficiency: Sunlight exposure is a primary source of vitamin D. Low levels of vitamin D have been linked to depressive symptoms, and insufficient sunlight during winter can contribute to this deficiency.
- Genetic Factors: Some people are more genetically predisposed to experience SAD due to a family history of mood disorders or particular serotonin-transporter genes.
2. Symptoms of SAD
- Persistent low mood
- Loss of interest or pleasure in everyday activities
- Fatigue and low energy despite adequate sleep
- Increased appetite, particularly for carbohydrates, leading to weight gain
- Difficulty concentrating and making decisions
- Social withdrawal and increased irritability
- In severe cases, thoughts of self-harm or suicide may occur.
3. Effective Strategies for Managing SAD Symptoms
3.1. Light Therapy (Phototherapy)
- What It Is: Light therapy involves exposure to a bright light (at least 10,000 lux) that mimics natural sunlight. This is usually done with a lightbox for 20-60 minutes each morning.
- How It Helps: Light therapy can help realign circadian rhythms and reduce melatonin production, improving alertness and mood.
- Effectiveness: Studies suggest light therapy can improve symptoms in up to 85% of people with SAD within a week or two.
3.2. Cognitive Behavioral Therapy (CBT)
- What It Is: CBT is a structured, short-term form of psychotherapy focused on identifying and changing negative thought patterns.
- How It Helps: CBT helps individuals challenge and alter negative thoughts related to the season, breaking the connection between dark days and feelings of hopelessness.
- Effectiveness: Research has found CBT tailored for SAD (CBT-SAD) to be effective in reducing symptoms both in the short term and in preventing recurrence.
3.3. Physical Exercise
- Why It Works: Exercise releases endorphins, which act as natural mood lifters. Regular physical activity also improves sleep, reduces anxiety, and provides structure to daily routines.
- Types of Exercise: Aerobic exercises such as walking, cycling, and swimming are particularly beneficial. Exercising outdoors, even on cloudy days, can also provide natural light exposure.
3.4. Diet and Nutrition
- Avoiding Carbohydrate Cravings: SAD often leads to an increased craving for carbohydrates. A balanced diet with complex carbohydrates (whole grains) and protein-rich foods can stabilize blood sugar levels and mood.
- Supplementing with Vitamin D: Because sunlight exposure is limited in winter, taking a vitamin D supplement can help mitigate deficiency-related mood dips.
- Omega-3 Fatty Acids: Found in fish and flaxseed, omega-3s are known to support brain health and reduce symptoms of depression.
3.5. Social Connection and Support
- Importance of Social Engagement: Social withdrawal is common with SAD, but engaging with friends and family can significantly alleviate symptoms. Support groups and social gatherings provide emotional support and combat isolation.
- Therapeutic Support Groups: Group therapy sessions tailored to individuals with SAD can be a valuable resource, as members share coping strategies and provide mutual encouragement.
3.6. Mindfulness and Relaxation Techniques
- Mindfulness Practices: Meditation and mindfulness exercises help to reduce stress and improve focus, helping individuals maintain resilience against mood fluctuations.
- Guided Relaxation: Techniques such as deep breathing and progressive muscle relaxation can help manage anxiety and improve mood during winter.
3.7. Structured Daily Routine
- Benefits: Establishing a consistent routine helps create structure in days that may otherwise feel directionless and gloomy.
- Morning Sunlight Exposure: Maximize exposure to natural sunlight by scheduling outdoor activities during daylight hours, especially in the morning.
- Sleep Hygiene: Setting regular wake-up and bedtime hours, avoiding caffeine in the afternoon, and limiting blue light exposure before bed can improve sleep quality, which is essential for managing SAD symptoms.
3.8. Medication
- SSRIs: Selective serotonin reuptake inhibitors (SSRIs) are commonly prescribed for SAD when symptoms are severe or unresponsive to other treatments. These medications increase serotonin levels, helping to elevate mood and reduce anxiety.
- Bupropion (Wellbutrin): The FDA has approved this antidepressant specifically for treating SAD, particularly for its ability to prevent relapse.
4. Preventative Strategies for SAD
- Early Light Therapy: Beginning light therapy sessions in early fall before symptoms fully set in can help reduce the severity of SAD.
- Psychotherapy: Regular CBT sessions can build resilience to manage negative thoughts and prevent worsening of symptoms.
- Active Lifestyle: Maintaining an active lifestyle year-round, including outdoor time and physical exercise, can reduce the impact of winter on mood.
5. Importance of Early Diagnosis and Individualized Treatment
- Early diagnosis and a personalized approach are essential since SAD manifests differently across individuals. Some people respond better to light therapy, while others might need a combination of therapies and medications.
SAD is a complex disorder that arises from a blend of biological, psychological, and environmental factors. By combining lifestyle adjustments with therapeutic interventions like light therapy, CBT, and possibly medication, individuals can manage their symptoms and maintain a higher quality of life throughout the winter months.
Learn More
Dealing with Anxiety Triggers: Managing Relationships with Family Members who trigger our own anxiety: Some suggested steps to take and how to communicate when you feel the need to distance yourself or avoid interaction with them.
Living with anxiety can be challenging on its own, but navigating relationships with family members who trigger that anxiety adds an extra layer of complexity. Unlike casual acquaintances or coworkers, family members are often deeply integrated into your life, making avoidance more difficult and potentially damaging to family bonds. However, there are ways to address these relationships and manage your anxiety while maintaining boundaries and open communication.
This article explores the emotional challenges of interacting with family members who exacerbate anxiety, provides steps to cope, and offers practical advice on how to communicate your needs effectively. Understanding these techniques can help you maintain your mental well-being while minimizing tension within the family.
Understanding How Family Can Trigger Anxiety
Before diving into solutions, it’s essential to identify why family members may provoke feelings of anxiety. These reasons vary greatly depending on personal history, family dynamics, and individual triggers. Some common causes include:
- Unresolved Past Conflicts: Recurring conflicts from the past can leave emotional scars that resurface during interactions.
- Unrealistic Expectations: Families often place expectations on members to behave, achieve, or live up to certain standards, leading to pressure and anxiety.
- Lack of Boundaries: Overly invasive or controlling family members can make one feel suffocated, stripping away a sense of autonomy.
- Emotional Manipulation: Family members who use guilt or emotional manipulation can induce stress and anxiety, creating a toxic atmosphere.
- Family Roles and Dynamics: Traditional family roles or a history of dysfunction may perpetuate toxic dynamics that cause anxiety.
- Frequent Criticism or Judgment: Family members who frequently criticize or judge you can trigger feelings of inadequacy, leading to social anxiety and withdrawal.
Identifying the specific triggers within your family dynamic is crucial. Once you’re aware of these, you can begin addressing them with clear boundaries and communication strategies.
Steps to Take When Dealing with Family-Related Anxiety
When faced with family-induced anxiety, it’s important to approach the situation with care. Rather than impulsively reacting or permanently severing ties, consider these thoughtful steps to manage your mental health and maintain your relationship with your family members:
- Recognize Your Triggers Start by identifying which situations or behaviors from family members trigger your anxiety. Is it certain conversations, comments about your life, or particular family gatherings? Understanding what sets you off can help you take proactive measures to address the issue and plan how to respond before encountering similar situations again.
- Set Healthy Boundaries Once you’ve pinpointed the sources of anxiety, the next step is to set boundaries. Boundaries are crucial for maintaining emotional health, especially with family. Whether it’s limiting the time you spend with them or making certain topics off-limits in conversations, healthy boundaries prevent you from feeling overwhelmed.
For example, if family members often criticize your life choices, politely let them know you won’t entertain discussions on those subjects. You can say, “I appreciate your concern, but I would prefer not to talk about my job or relationships at this time.”
- Limit Exposure to Toxic Situations While it might be impossible to cut off contact with family members completely, reducing your exposure to toxic situations can help. Skip gatherings that make you anxious, or spend less time with people who trigger your anxiety. Focus on protecting your mental health, even if it means saying no to certain events.
- Practice Self-Care Engaging in self-care is crucial to managing anxiety, particularly when dealing with family triggers. This could involve physical activities like yoga or exercise, journaling your emotions, meditating, or simply giving yourself a break from toxic conversations. Self-care isn’t selfish—it’s a necessary part of maintaining your well-being.
- Seek Professional Support If family dynamics are too overwhelming, seeking professional guidance through therapy can be immensely helpful. Therapists can help you process emotions, develop coping strategies, and teach you how to handle difficult family relationships without sacrificing your mental health. Cognitive Behavioral Therapy (CBT) is a particularly effective treatment for anxiety triggered by familial interactions.
Effective Communication Strategies for Setting Boundaries
Communicating your boundaries with family members can be challenging, especially when they are not used to you asserting your needs. Clear, respectful communication is key to maintaining your mental health and preserving family relationships.
- Be Direct and Clear When discussing your boundaries, be as clear as possible. Avoid vague language that could be misinterpreted. For example, instead of saying, “I don’t want to talk about work,” you could say, “I’m currently stressed about work, and I would like to avoid discussing it during family gatherings.”
- Use “I” Statements Frame your concerns using “I” statements, which focus on your feelings rather than placing blame. For example, “I feel anxious when conversations get too heated, and I’d like to change the subject when that happens,” instead of, “You always make me anxious when we argue.” This approach prevents defensiveness and keeps the conversation solution-focused.
- Remain Calm and Respectful Even if the conversation feels tense, try to stay calm and respectful. Losing your temper or reacting with hostility may escalate the situation and reinforce negative family dynamics. Approach the discussion with the goal of resolution, not confrontation.
- Be Consistent with Your Boundaries Once you’ve set a boundary, it’s important to enforce it consistently. Family members may test your limits, but standing firm will show them that you’re serious about protecting your well-being. For example, if you’ve asked them not to bring up a certain topic and they do, gently remind them, “I’ve asked that we don’t discuss this subject.”
- Know When to Walk Away If family members continue to push your boundaries or create anxiety despite your best efforts, it may be necessary to distance yourself temporarily or walk away from the conversation. Protecting your mental health should be your top priority, even if it means stepping away from difficult family interactions.
When Avoiding Interaction is Necessary
There are instances when avoiding or limiting contact with certain family members is necessary to protect your mental health. Some relationships are too toxic or damaging to manage on a day-to-day basis, even with boundaries in place. Here are some situations where avoidance might be a viable option:
- Emotional or Physical Abuse If a family member is emotionally manipulative, verbally abusive, or physically threatening, it’s essential to distance yourself from them. No relationship, family or otherwise, is worth sacrificing your safety or mental well-being.
- Persistent Boundary Violations If you’ve set clear boundaries and they are consistently ignored or violated, it may be time to minimize or avoid contact. Repeated boundary violations demonstrate a lack of respect for your needs and mental health.
- Unwillingness to Compromise Family dynamics are healthiest when there is mutual respect and a willingness to compromise. If a family member refuses to meet you halfway and continues to act in ways that trigger anxiety, limiting interactions may be the best solution for your well-being.
- Toxic Environments If the family environment is consistently toxic—whether due to constant arguing, manipulation, or negativity—consider reducing your exposure to it. Your mental health should come before maintaining obligatory ties to unhealthy family dynamics.
Coping Mechanisms for Anxiety During Family Gatherings
Sometimes, avoiding family gatherings entirely may not be possible or desired. In those cases, it’s important to have coping mechanisms in place to manage your anxiety during interactions with family members who trigger you.
- Have an Exit Plan Before attending a family gathering, establish an exit plan in case things become too overwhelming. This could involve leaving early or taking short breaks to step outside, calm down, and refocus.
- Breathe and Ground Yourself Practice deep breathing or grounding techniques when anxiety starts to rise. Breathing exercises can help slow your heart rate and bring you back to the present moment, keeping anxiety at bay during triggering interactions.
- Focus on Supportive Family Members At family events, try to gravitate towards those who provide comfort and support rather than those who trigger anxiety. Spend your time with people who uplift and encourage you rather than those who make you feel drained.
- Limit Alcohol and Caffeine Both alcohol and caffeine can exacerbate anxiety, making you more susceptible to stress. Limiting your intake of these substances can help keep your anxiety levels manageable during family gatherings.
- Prepare Responses Ahead of Time If you know certain topics or comments will trigger anxiety, plan responses ahead of time. Having pre-prepared statements can help you navigate difficult conversations more smoothly and feel more in control.
Final few words: Managing Family Dynamics and Prioritizing Mental Health
Dealing with anxiety, especially when triggered by close family members, can be a painful and exhausting experience. However, by taking proactive steps—recognizing triggers, setting boundaries, communicating clearly, and prioritizing your well-being—you can manage these relationships in a way that protects your mental health without completely severing ties.
Remember, it’s okay to step back from relationships that negatively impact you. You are not obligated to tolerate behaviors that trigger anxiety, even from family members. By focusing on self-care, boundary setting, and seeking professional support when necessary, you can maintain a healthier and more balanced approach to family dynamics while prioritizing your mental health.

